Cranial Nerve Exam: A Comprehensive Guide
This guide details the twelve paired cranial nerves originating from the brain, crucial for functions like vision, taste, and facial movement.
These nerves transmit sensory and motor data, bypassing the spinal cord for rapid communication, and are essential for neurological assessments.
Cranial nerves represent a vital component of the neurological examination, offering a direct assessment pathway to the brainstem and peripheral nervous system functionality. These twelve paired nerves emerge directly from the brain, unlike most other nerves which relay signals through the spinal cord. This unique characteristic allows for a rapid transmission of both sensory and motor information, impacting diverse functions.

Understanding their roles – encompassing smell, vision, eye movement, facial sensation and expression, hearing, balance, taste, swallowing, speech, and control of shoulder and tongue movements – is paramount. A comprehensive cranial nerve exam isn’t merely a checklist; it’s a nuanced evaluation that can pinpoint the location and nature of neurological deficits. Resources like downloadable PDFs often serve as valuable guides for clinicians, detailing examination techniques and interpretive strategies. These resources emphasize a systematic approach, ensuring no nerve is overlooked during the assessment process.
The exam allows for focused evaluation of the brainstem.
The 12 Pairs of Cranial Nerves
The twelve cranial nerves are designated by Roman numerals, each possessing unique functions and pathways. I – Olfactory (smell), II – Optic (vision), III – Oculomotor (eye movement), IV – Trochlear (eye movement), V – Trigeminal (facial sensation & muscles), VI – Abducens (eye movement), VII – Facial (expression & taste), VIII – Vestibulocochlear (hearing & balance), IX – Glossopharyngeal (taste & swallowing), X – Vagus (speech, swallowing, visceral function), XI – Accessory (shoulder & neck movement), and XII – Hypoglossal (tongue movement).
These nerves are symmetrically arranged, primarily serving the head and neck, with the vagus nerve extending into the chest and abdomen. Detailed cranial nerve exam PDFs often include mnemonics to aid in memorization of nerve names and functions. Understanding each nerve’s specific role is crucial for accurate interpretation of examination findings. A systematic approach, guided by these resources, ensures a thorough assessment of neurological integrity. The exam allows one to examine the brainstem, as cranial nerves exit the CNS.
Importance of the Cranial Nerve Exam
The cranial nerve exam is a fundamental component of the neurological assessment, providing valuable insights into the function of the brainstem and surrounding structures. It aids in localizing lesions affecting these nerves, helping to differentiate between central and peripheral nervous system disorders. Comprehensive cranial nerve exam PDFs emphasize the exam’s utility in diagnosing conditions like stroke, tumors, multiple sclerosis, and Bell’s palsy.
A thorough examination can reveal subtle deficits that might otherwise be missed, enabling early intervention and improved patient outcomes. It’s crucial for evaluating patients with headaches, dizziness, vision changes, facial weakness, or swallowing difficulties. Mastering this exam, as detailed in clinical guides, allows clinicians to efficiently assess neurological function and guide further diagnostic testing. The exam’s sensitivity and specificity make it an indispensable tool in neurological practice, offering a direct assessment of brainstem integrity.
Detailed Examination Techniques
Detailed PDFs outline systematic testing for each cranial nerve, covering olfactory, optic, and oculomotor functions. Precise methods ensure accurate assessment of sensory and motor pathways.
I. Olfactory Nerve (Smell) – Testing Methodology
Assessing the olfactory nerve (CN I) involves testing a patient’s ability to identify common odors, utilizing non-irritating substances like coffee, vanilla, or peppermint. Crucially, each nostril is tested separately, with the patient’s eyes closed to eliminate visual cues.
PDF guides emphasize presenting the odorant to one nostril while the patient occludes the other. The examiner should ask the patient to identify the smell, or if they can detect any smell at all. It’s vital to avoid strong or potentially irritating substances that could stimulate the trigeminal nerve instead.

Documentation should include whether the sense of smell is present, diminished, or absent in each nostril. Anosmia refers to a complete loss of smell, while hyposmia indicates a reduced ability to detect odors. PDF resources often include standardized scoring systems for olfactory testing, ensuring consistent and comparable results. Careful attention to technique minimizes false positives and negatives during this essential component of the cranial nerve examination.
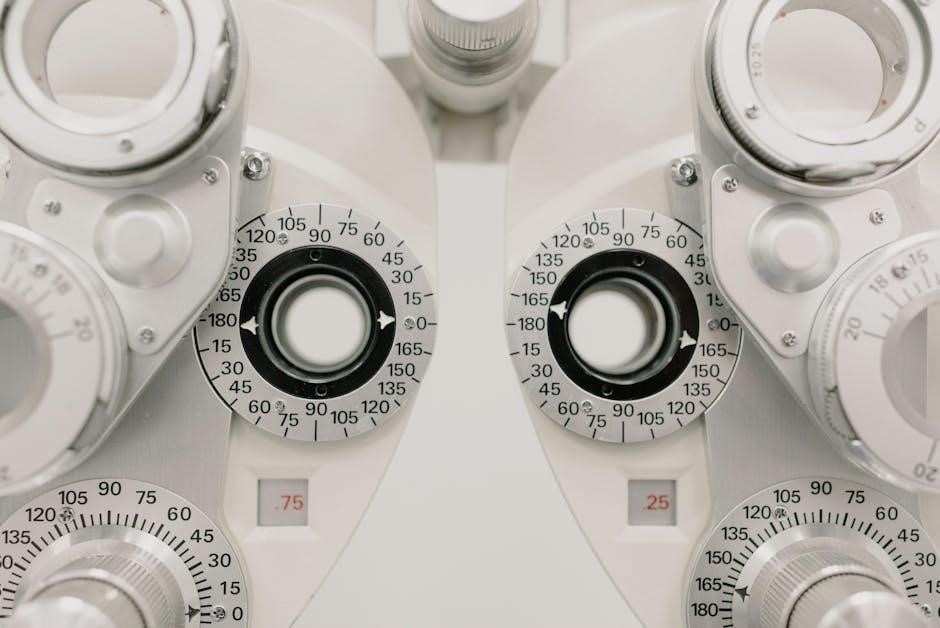
II. Optic Nerve (Vision) – Visual Acuity & Fields
Evaluating the optic nerve (CN II) begins with assessing visual acuity, typically using a Snellen chart at a standard distance (20 feet). Each eye is tested individually, both with and without corrective lenses, documenting the best-corrected visual acuity.
PDF guides detail the importance of accurately recording the results, such as 20/20, 20/30, or worse. Following acuity testing, visual fields are assessed by confrontation, comparing the patient’s peripheral vision to the examiner’s.
Formal perimetry can be used for more precise field mapping. PDF resources often illustrate how to perform accurate confrontation testing, emphasizing the importance of consistent stimulus presentation. Defects in the visual field, like scotomas or hemianopsia, can indicate optic nerve damage or lesions along the visual pathway. Careful documentation of any field deficits is crucial for diagnosis and monitoring.
III. Oculomotor, IV. Trochlear, & VI. Abducens Nerves (Eye Movement) – Assessment
Assessing oculomotor (III), trochlear (IV), and abducens (VI) nerves involves observing extraocular movements. The examiner instructs the patient to follow a moving target, like a finger or penlight, in all directions of gaze – up, down, left, right, and diagonally. PDF guides emphasize looking for smooth, coordinated movements.
Nystagmus, or involuntary rhythmic eye movements, should be noted, along with any limitations in range of motion. Ptosis (drooping eyelid) can indicate oculomotor nerve dysfunction.
The “H” test, tracing an “H” shape with the target, efficiently assesses all six cardinal gazes. PDF resources often include diagrams illustrating the muscles innervated by each nerve and the expected movements. Diplopia (double vision) is a key symptom, and its characteristics – monocular or binocular – help localize the lesion. Accurate observation and documentation are vital for a comprehensive neurological evaluation.
V. Trigeminal Nerve (Facial Sensation & Muscles) – Sensory & Motor Components
The trigeminal nerve (V) assessment divides into sensory and motor components. Sensory testing evaluates light touch, pain, and temperature sensation across the three branches: ophthalmic (V1), maxillary (V2), and mandibular (V3). PDF guides detail using a cotton wisp or sharp/dull object, comparing bilaterally. Decreased sensation or hyperesthesia suggests dysfunction.
Motor function is tested by palpating the masseter and temporalis muscles during clenching. Weakness indicates involvement. The corneal reflex – touching the cornea with cotton – tests V1 afferent limb and VII efferent.
Jaw jerk reflex, elicited by tapping the chin, assesses V3. PDF resources often include dermatome maps for precise localization. Facial pain, numbness, or weakness are key symptoms. Thorough assessment helps differentiate between central and peripheral lesions, guiding further investigation.

Further Cranial Nerve Assessments
Detailed PDF guides expand on initial testing, focusing on nerves VII-XII. These assessments evaluate facial expressions, hearing, balance, swallowing, speech, and tongue movement comprehensively.
VII. Facial Nerve (Facial Expression & Taste) – Examination Protocol
Assessing the facial nerve (VII) involves evaluating both its motor and sensory-taste functions. Begin by observing the patient’s face for symmetry at rest. Ask the patient to perform a series of facial movements, including raising eyebrows, closing eyes tightly (checking for complete closure and noting any lag on either side), puffing out cheeks, smiling, and showing teeth.
Carefully observe for any weakness or asymmetry during these maneuvers. Note any flattening of the nasolabial fold, drooping of the mouth, or difficulty closing the eye.
Taste assessment is performed by applying small amounts of sweet, sour, salty, and bitter solutions to the anterior two-thirds of the tongue on each side, using cotton swabs. The patient should identify the taste.
PDF resources often include diagrams illustrating facial nerve pathways and potential lesion locations. Document any deficits observed during both the motor and taste components of the examination, as these can indicate facial nerve dysfunction due to various causes.
VIII. Vestibulocochlear Nerve (Hearing & Balance) – Testing Procedures
Evaluating the vestibulocochlear nerve (VIII) requires assessing both auditory and vestibular functions. Begin with a hearing assessment using whispered voice tests, comparing the patient’s ability to hear sounds equally in both ears. Weber and Rinne tests are then performed to differentiate between conductive and sensorineural hearing loss.
For the Weber test, a vibrating tuning fork is placed on the midline of the head; a patient with conductive hearing loss will lateralize the sound to the affected ear. The Rinne test compares air and bone conduction – normal hearing exhibits air conduction > bone conduction.
Vestibular function is assessed through observation of balance and coordination, and potentially with maneuvers like the Romberg test. PDF guides often detail specific caloric testing procedures, involving irrigation of the ear canal with cold water to stimulate the vestibular system.
Document any hearing deficits or balance disturbances, as these can indicate dysfunction of the vestibulocochlear nerve.
IX. Glossopharyngeal Nerve (Taste & Swallowing) – Clinical Evaluation
Assessing the glossopharyngeal nerve (IX) involves evaluating taste sensation on the posterior third of the tongue, swallowing function, and the gag reflex. Begin by testing taste using sugar or salt solutions, noting any asymmetry. PDF resources emphasize careful application to avoid contamination between solutions.
Swallowing is assessed by observing the patient drink water, looking for any signs of dysphagia, such as coughing or choking. The gag reflex is elicited by gently stimulating the posterior pharynx with a tongue depressor; a symmetrical response is expected.
Carefully document any deficits in taste, difficulty swallowing, or an absent/asymmetrical gag reflex. These findings can indicate damage to the glossopharyngeal nerve or related brainstem structures.
Clinical guides often include detailed diagrams illustrating the anatomical pathways and potential lesion locations associated with glossopharyngeal nerve dysfunction.
X. Vagus Nerve (Speech, Swallowing, & Visceral Function) – Examination Steps
Evaluating the vagus nerve (X) requires assessing speech articulation, swallowing, and observing for signs of autonomic dysfunction. Begin by listening to the patient’s speech for hoarseness or nasal quality, indicative of vocal cord paralysis. PDF guides highlight the importance of noting any changes in voice volume or pitch.
Swallowing is assessed similarly to the glossopharyngeal nerve, observing for dysphagia. Examine the uvula and soft palate for symmetry and elevation during phonation (“ah” sound). Deviation suggests vagal nerve weakness.
Autonomic function is indirectly assessed by observing heart rate and blood pressure changes during maneuvers like the Valsalva maneuver. Detailed cranial nerve exam PDFs often include checklists for systematic assessment.
Document any vocal cord paralysis, swallowing difficulties, or autonomic abnormalities, as these can pinpoint vagal nerve involvement.

Completing the Exam & Interpretation
A systematic cranial nerve exam, often detailed in PDF guides, aids in pinpointing neurological issues. Careful documentation and correlation with patient history are essential for accurate diagnosis.
XI. Accessory Nerve (Shoulder & Neck Movement) – Motor Strength Assessment
Assessing the accessory nerve (CN XI) focuses on evaluating motor strength in the sternocleidomastoid and trapezius muscles. These muscles are responsible for head and shoulder movements, and weakness can indicate nerve dysfunction. A comprehensive cranial nerve exam PDF will detail these steps.
To test the sternocleidomastoid, have the patient turn their head against resistance. Note any weakness or asymmetry. For the trapezius, ask the patient to shrug their shoulders against resistance, observing for diminished strength on either side. Also, assess the ability to extend the head against resistance, testing the upper trapezius fibers.

Palpate both muscles for atrophy or fasciculations, which can suggest chronic nerve damage. Document the strength grading using a standardized scale (0-5). Remember that unilateral weakness may indicate a lesion affecting the accessory nerve itself, while bilateral weakness could suggest a more widespread neurological issue. Detailed PDF resources often include illustrative diagrams and specific grading criteria.
XII. Hypoglossal Nerve (Tongue Movement) – Tongue Protrusion & Strength
Evaluating the hypoglossal nerve (CN XII) involves observing tongue movement, both at rest and during function. A thorough cranial nerve exam PDF will guide clinicians through this process. Begin by asking the patient to protrude their tongue, noting any deviation to one side, asymmetry, or fasciculations. Deviation suggests weakness on the opposite side.
Next, assess tongue strength by having the patient push their tongue against their cheek against resistance. Repeat on both sides, observing for weakness. Also, ask the patient to move their tongue from side to side and up and down, looking for limitations in range of motion or coordination.
Document any observed abnormalities, including the degree of deviation, strength grading (0-5), and presence of fasciculations. A comprehensive PDF resource will often include images illustrating normal and abnormal findings, aiding in accurate assessment and diagnosis.

Interpreting Abnormal Findings & Associated Conditions
A comprehensive cranial nerve exam PDF is crucial for accurate interpretation of findings. Isolated cranial nerve deficits often pinpoint localized lesions, while multiple deficits suggest broader neurological issues. For example, facial droop (VII) and tongue deviation (XII) could indicate a stroke.
Understanding associated conditions is vital. Tumors, particularly those at the skull base, frequently compress cranial nerves. Multiple sclerosis can cause demyelination affecting nerve transmission. Infections, like Bell’s palsy (VII), present with facial paralysis. Trauma can directly damage nerves.
The PDF should detail differential diagnoses based on patterns of deficits. Thorough documentation, including specific nerve involvement and associated symptoms, guides further investigation – MRI, CT scans, or specialized neurological testing – to confirm the diagnosis and determine appropriate treatment strategies.